Black heritage donors giving blood in record numbers
More people than ever before of Black African and Black Caribbean heritage are saving lives by giving blood – but more donations are urgently needed to help sickle cell patients who depend on ethnically matched blood.
The number of regular donors of Black heritage reached an all-time high of almost 20,000 (1) in the year to April while a further 7,427 (2) gave blood for the first time - also a record. Both figures have doubled since 2017 when the NHS began appealing for Black heritage donors (3).
But the shortage remains critical. This year the NHS needs 12,000 new Black heritage donors to meet the growing demand for ethnically matched blood for sickle cell patients who need regular transfusions to stay alive.
Today, at the start of National Blood Week, NHS Blood and Transplant is rolling out a major new campaign celebrating donors and appealing for new donors to join the team of ‘Giving Types’, particularly those of Black heritage.
And to launch the campaign a 20ft mural depicting five inspirational blood donors of Black heritage from across England is being unveiled today in London’s Stockwell Hall of Fame. Created by Black-British street artist Dreph, the striking mural will be on display to the public for the duration of National Blood Week.
Youth worker Ronald Clarke from Greater Manchester is one of the donors featured in the mural. He is passionate about blood donation and believes it is a great and easy way to give something back to the community.
How your donation could help
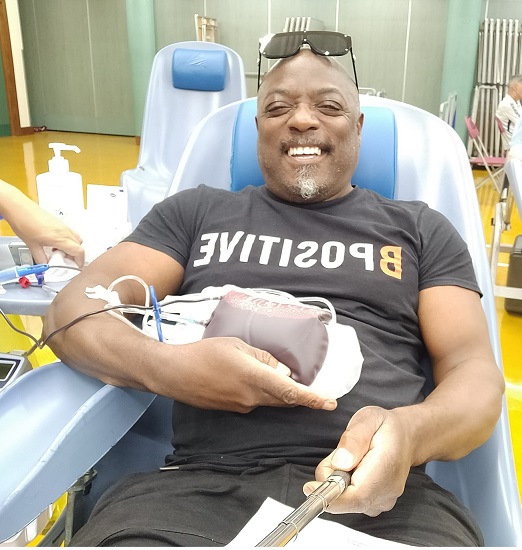 Ronald is a member of the B Positive Choir and in 2018 made it to the finals of Britain’s Got Talent, allowing them a national platform to spread the message about the lifesaving power of blood donation.
Ronald is a member of the B Positive Choir and in 2018 made it to the finals of Britain’s Got Talent, allowing them a national platform to spread the message about the lifesaving power of blood donation.
Ronald, 63, said:
"I've been donating blood for a few decades now. I enjoy the experience as it's a quick process and I know it'll always be of benefit to someone. I like being able to go with friends to donate as it's a way of sharing a positive experience with a friend."
Sickle cell is more prevalent in people of Black heritage and blood from a donor of the same ethnicity provides the best treatment. Because the NHS can’t collect enough some patients need to be treated with the universal O Negative blood type. This is clinically safe but can put them at risk of serious complications and makes it even harder in the long term to find blood they can receive.
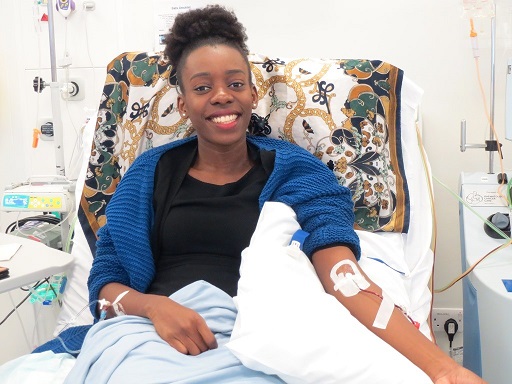 Mary Adeturinmo, 30, from London, needs all her blood replaced by donor blood every four weeks due to sickle cell. Since starting the treatment at the age of 23 she has experienced fewer episodes of excruciating pain, known as a sickle cell crisis.
Mary Adeturinmo, 30, from London, needs all her blood replaced by donor blood every four weeks due to sickle cell. Since starting the treatment at the age of 23 she has experienced fewer episodes of excruciating pain, known as a sickle cell crisis.
Mary, an outreach officer for NHS Blood and Transplant, said:
"Although many in the Black community are aware of sickle cell, it is not widely known that a transfusion is more successful when the donated blood is from someone with a similar ethnic heritage."
"Donated blood helps me live life to the fullest. For some sickle cell patients, it’s the difference between life and death. But we need more donations from the Black community to give us the best chance."
The Giving Type
The new campaign encourages 'Giving Types' - people who give in big and little ways, whether that be giving up a seat on a train, for example, or raising money for charity - to consider becoming a blood donor.
The campaign will run over three months and includes a TV advert as well as adverts on radio, social media and out of home advertising.
Dr Jo Farrar, Chief Executive of NHS Blood and Transplant, said:
"It is fantastic that more people of Black heritage than ever before are saving lives by giving blood. But we urgently need more regular Black heritage donors so that sickle cell patients can receive the best treatment."
"This National Blood Week, please join our amazing team of 'Giving Types'. Giving blood is safe and easy and in just one hour you can save up to three lives. Our permanent donor centres in towns and cities are great places for your first donation."
Health Minister Neil O’Brien said:
"NHSBT has made huge progress in recruiting donors of Black heritage, with the number of regular donors and first-time donors doubling since 2017."
"But more people are urgently needed to meet the growing demand to treat sickle cell patients, who need regular blood transfusions to stay alive."
"I want to thank NHSBT and praise the generosity of those who give blood for making these life-saving, record figures possible and I urge everyone to consider donating blood."
How you can help
This year the NHS needs 140,000 new blood donors to grow and diversify the base of donors so blood and blood products can continue to be supplied to hospitals. Around 9,000 new plasma donors are also needed.
Blood donation can now save even more lives because the plasma can be recovered from the blood and made into a medicine which treats more than 50 disorders such as Kawasaki disease and myasthenia gravis.
Become a blood donor and book your first appointment via the GiveBloodNHS app or through our website. If you can’t find an appointment straight away please book for further in the future. Your blood will still help to save lives then.
Press release notes
- An existing donor who has donated at least once during this period. Between April 2022 and March 2023 there were 19,300 regular donors of Black heritage and 799,000 regular donors of all ethnicities. This compares with 9,870 and 852,000 respectively in 2016/17.
- 7,427 people of Black heritage gave blood for the first time between April 2022 and March 2023 compared with 3,315 in 2016/17.
- NHS Blood and Transplant began appealing for Black heritage donors in 2017 to meet the growing demand for ethnically matched blood following a change in the way the NHS treats sickle cell. In the past, many patients had intermittent top up blood transfusions. However, more patients have been identified as benefiting from regular full exchange transfusions. This is where all their deformed red blood cells are gradually filtered out and replaced with healthy donor blood. This complete blood transfusion requires a lot more blood, and that blood must be matched to prevent the risk of transfusion reactions building up over time.
