Collaborative report into evidence on gay and bisexual men and blood donation still due in 2020
Update! New information from the FAIR group is now available. Read the FAIR group update here
The FAIR steering group exploring whether some gay and bisexual men might be able to donate blood without a deferral is still hoping to report its’ findings before the end of 2020.
The work has been delayed by the coronavirus pandemic but it is progressing and the group plans to submit a report before the end of the year.
 FAIR (For the Assessment of Individualised Risk) was set up at the beginning of 2019 at the request of the Department of Health and Social Care.
FAIR (For the Assessment of Individualised Risk) was set up at the beginning of 2019 at the request of the Department of Health and Social Care.
The steering group includes representatives from the four UK blood services, LGBT+ groups, medical and scientific experts, and patient and donor representatives (1).
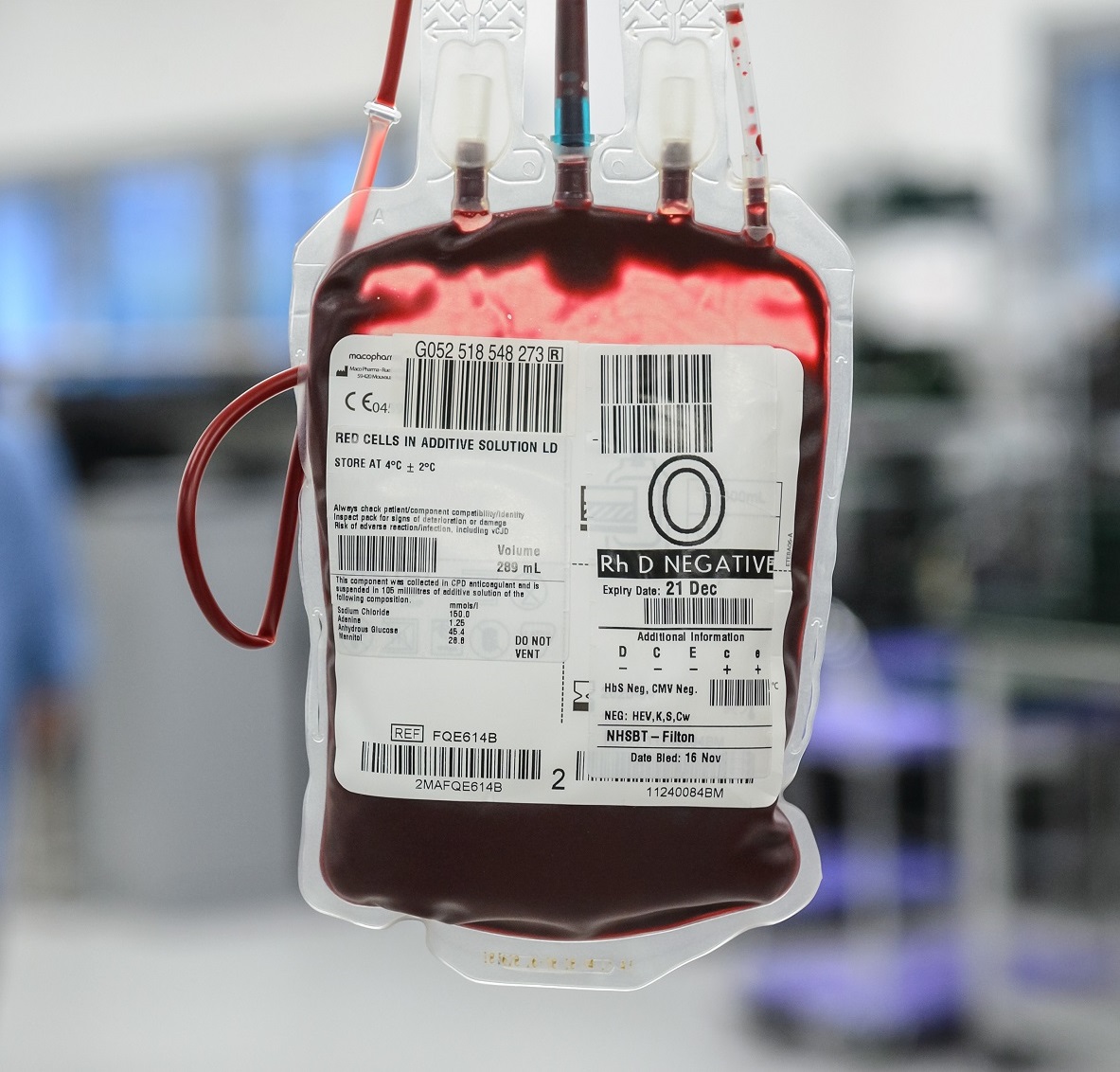
It is exploring whether there is sufficient evidence to change the current blood donor selection policy. Currently, a man who has had sex with a man is deferred from donating blood for three months.
Blood donation guidelines are set by the Department of Health and Social Care based on recommendations from the Advisory Committee on the Safety of Blood, Tissues and Organs (SaBTO).
The current three month deferral uses ‘population based risk’ and the FAIR work could lead to the use of a more individualised assessment of risk, whilst still maintaining the safety of the blood supply. The change might enable some men who have sex with men but who are deferred under the current policy, to give blood.
FAIR is taking a collaborative, evidence led approach. This has included conducting focus groups with gay and bisexual men. Existing public health data and research is being examined to scope how best to identify individuals at high and low risk of infections. Thousands of current and potential new blood donors are being surveyed to examine how people would respond to possible new and more detailed questions about their sexual behaviours. A mixture of workshops, focus groups and interviews are being held with groups such as blood donation session staff, current blood donors and potential new donors.
Currently all blood donors are asked a series of questions on travel, health, tattoos, sexual behaviour and more, to help assess how safe it is for them to donate, and how safe it is for someone to receive their blood. A central part of FAIR’s work is considering which new questions could successfully be added to identify donors, including men who have sex with men, at lower risk of acquiring certain infections that can be transmitted through blood (2)(3)(4)(5).
Dr Su Brailsford, the chair of FAIR, who holds senior roles at both NHS Blood and Transplant and Public Health England, said: “We are all committed to equality, diversity and inclusion and we are pleased to be working collaboratively with other organisations on this important issue.
“We need a donor selection system that is safe and can also cope with large numbers of people. We need to understand which questions are most relevant to assessing risk and whether there are some questions which might put people off donating.
“This work takes time and we need to make sure everything we do is based on good evidence with patient safety as the number one priority.
“We appreciate that any deferral is disappointing if you want to save lives by giving blood and recognise that people want to be considered as individuals as much as possible. We want to give as many people as possible the opportunity to donate whilst continuing to ensure the safety of both the blood supply and those patients who receive blood.”
Debbie Laycock, Head of Policy at Terrence Higgins Trust, said: “As a member of the FAIR steering group, we are pleased that the important work of this group is progressing and that its recommendations will be released this year.
“We have long campaigned for a blood donation system that better reflects the realities of sexually transmitted infections. That’s why we welcomed the reduction in the deferral period to three months for those who are gay and bisexual men, and we will continue to support this work around exploring an individual risk assessment.”
A Stonewall spokesperson said: “We’re very pleased to be working with NHSBT and other partners on this vital project exploring ways to stop the blanket restriction against gay and bi men looking to donate blood. Working towards introducing a system of individualised risk assessment is a crucial part of allowing people who want to save lives to safely donate blood.”
- FAIR aims to submit a report to the Advisory Committee on the Safety of Blood, Tissues and Organs (SaBTO) by the end of 2020.
- NHSBT’s LGBT+ Network has a page outlining the guidance on blood, organ, stem cell and tissue donation if you are LGBT+
- The membership includes NHS Blood and Transplant, Scottish National Blood Transfusion Service, the Welsh Blood Service, the Northern Ireland Blood Transfusion Service, Public Health England, the University of Nottingham, the National Aids Trust (NAT), Stonewall, Freedom to Donate, Terrence Higgins Trust (THT), patient and donor representatives, and experts in epidemiology, virology and psychology.
- The Government sets blood donor selection criteria based on expert advice from the Advisory Committee on the Safety of Blood, Tissues and Organs (SaBTO). In 2017, the UK introduced a world-leading blood donation policy reducing the deferral to three months since last sexual contact for MSM. In many parts of the world the deferral is 12 months or longer and in some areas men who have sex with men are asked not to donate at all.
- Anyone can acquire a blood-borne virus or a sexually transmitted disease, but some people have an increased risk of exposure. At a population level, men who have sex with men have higher rates of blood borne viruses and sexually transmitted diseases. Using protection like a condom or pre-exposure prophylaxis can reduce this risk, but it doesn’t always eliminate it. The deferral is set at three months because even the most sensitive tests cannot pick up early infections. Hepatitis B has the longest infection window of the blood borne viruses that are significant risks and the time is set at three months to protect against that infection window period.
- The current donor questionnaire includes questions on exposure to risk, based on the best available expert evidence. These questions cover many things including travel, tattoos, illness, and sexual behaviour. The questions are there to protect the health of the donor and the health of the person who will receive the blood.
- The COVID-19 convalescent plasma donation programme is covered by the same donor selection criteria. No additional deferrals were introduced for the programme.

